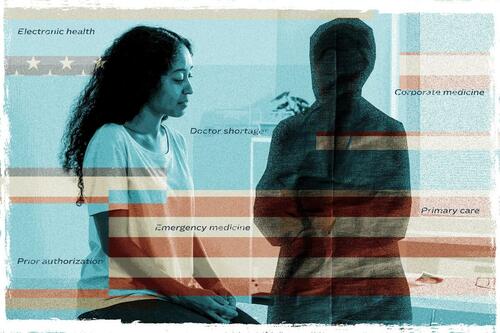
What’s Behind America’s Doctor Crisis?
Authorized by Autumn Spredemann via The Epoch Times (emphasis ours),
 (Illustration by The Epoch Times, Getty Images, Shutterstock)
(Illustration by The Epoch Times, Getty Images, Shutterstock)Securing an appointment to see a doctor in the United States is exacerbated byizing wellness care request and fever doctors. Many specializations are creatively affected by this trend, but primary care and emergency medicine are among the hardest hits.
The average wait time to see a doctor has increased since 2017 and continued to emergence after the request spice brought on by COVID-19. A survey conducted by AMN Healthcare in 2022 of 15 large metro markets revealed the average time to see a physics was 26 days—an 8 percent increase from 2017 and a 24 percent spice since 2004.
Staff constraints are besides felt in infirmary emergency departments. Nearly 140 million Americans visited a infirmary emergency department in 2021, based on data from the Centers for illness Control and Prevention. Of these, about 13 percent resulted in infirmary admission; while thousands waited hours to see a wellness care provider.
Consecently, Many patients leave before being seen by a doctor.
One survey analyzed more than 1,000 hospitals between 2017 and the end of 2021 and found something with the worst performance had 4.4 percent of the Emergency area patients leave before a medical evaluation was conducted. At the end of 2021, that number had hazard to upgrades of 10 percent.
Compounding the issue is that nearly half of the doctor population will scope retention age within the next 10 years and career burnout is hitting the remainder harder than ever, according to data from Association of American Medical Colleges.
Almost 50 percent of doctors study that they feel burned out, according to a 2024 Medicape report.
These are key factors driving America’s increasing Scarcity of doctors. doctor Three’s 2023 survey noted that the United States may have a shortage of 124,000 doctors by 2034. Within that shortfall, up to 48,000 will likely be lost from primary care, while the manufacture is projected to lose another 58,000 specialists, surgeons, and caregiver workers.
“This is definitely coming down the pipeline. It’s been coming for a long time, and we’re seeing this all across wellness care,” Emergency doctor Dr. Jared Ross told The Epoch Times.
Dr. Ross is besides president of Missouri-based Emergency Medical Services, Education & Consulting. He’s watched America’s wellness care individual crisis unfolded on the front lines and says the shortage of physicians is an old problem that’s reached a tipping point.
“We’ve talked about this for years. It’s nothing new. There’s been a number of attempted stop-gap measures that haven’t been all that successful,” he said.
 A individual walks past an 'Emergency Entrance' sign at Mount Sinai infirmary in fresh York City on Sept. 22, 2020. (Spencer Platt/Getty Images)
A individual walks past an 'Emergency Entrance' sign at Mount Sinai infirmary in fresh York City on Sept. 22, 2020. (Spencer Platt/Getty Images)Some of these provisional solutions include bringing in more practitioners from abroad countries, medical school debt insurance programs, expanding telehealth services, and expanding the number of resident physicist training supported by Medicare.
Dr. Ross has seen doctor shortages impact Emergency medicine but maintains primary care has “really strugled” to hold physicians.
This is critical for 2 reasons. 1 is due to the fact that wellness care demands in the United States are rising. The average number of times Americans visit a doctor per year by age group is 4 times for adults, 9 for infants, and 2 for children between the ages of 5 and 15, according to Vanguard Medical Group.
The another reason is due to what Dr. Ross called the “corporateization of medicine.”
“The problem is we have an insurance strategy that is simply a massive bureaucracy,“ he said.
During a fresh conference with another medical leaders, Dr. Ross said it was discussed how America has “really pushed distant from the model of conventional wellness care.”
There was a general consensus within the group that insurance companies have become besides powerful in medicine.
“The administrative burden or hassle, as many doctors describe it, is very disheartening,” Dr. William Schaffner, an infectious illness specialist at the Vanderbilt University Medical Center, told The Epoch Times.
Having worked in medicine for more than 40 years, Dr. Schaffner has witnessed it evolve into something “aggressively more complicated” as insurance companies expanded power over doctors. He says this trend became more noticeable by the 1990s.
“Doctors didn’t go to medical school in anticipation of arguing with insurance companies. It’s depressing and discouring,” Dr. Schaffner said.
In 2020, for the first time, 5 percent of U.S. physicians worked in private practice, according to the American Medical Association (AMA). Most have chosen to become employees of large medical groups, which has dramatically changed the paradigm of wellness care.
“The shift distant from independent practices is emblematic of the fiscal uncertainty and economical stress many physics face due to statutory payment cuts in Medicare, rising practice costs, and intuitive administrative burdens,” AMA president Dr. Jesse M. Ehrenfeld said in a 2023 statement.
 A wellness care professional suites up to enter a area in the ICU at Van Wert region infirmary in Van Wert, Ohio, on Nov. 20, 2020. (Megan Jelinger/AFP via Getty Images)
A wellness care professional suites up to enter a area in the ICU at Van Wert region infirmary in Van Wert, Ohio, on Nov. 20, 2020. (Megan Jelinger/AFP via Getty Images)Battling With Insurance
The decision from independent practice to medical group employer presents its own dilemma. Aside from increased patient loads, it has left doctors at the mercy of having to get prior approval from insurance companies to carry out a medical treatment or procedure.
This forces a quantity-over-quality approach to treatment, according to Dr. Ross.
Prior authorizations are “an absolute headache,” He said. Physicians are now stuck batting with a 3rd organization who created “as many roadblocks as possible due to the fact that they don’t want to pay out.”
Dr. Schaffner said it took “numbered telephone conversations” with an insurance supplier so a household associate could get a essential medical procedure done.
He said part of why it’s challenging is due to the fact that there needs to be a level of trust on the insurance company’s end. “It’s not just a formal relation that happens, but there besides should be a trust that develops with the benefits manager. It can take time,” Dr. Schaffner said.
Read more Here...
Tyler Durden
Fri, 05/10/2024 – 10:55